The Complete Guide to Thyroid Testing: Labs, Optimal Ranges & What They Mean
Years ago, I asked my doctor to run thyroid labs because I was hitting a wall: no matter how many high-intensity workouts I pushed through or how “clean” I ate, my body was stuck in weight loss resistance. What I didn’t know at the time is that diet culture itself — the overexercising, the restriction, the stress — can actually slow the thyroid and metabolism. (But that’s a conversation for another day.)
When I went back for the results, my doctor smiled, told me everything was “normal,” and sent me on my way.
Sound familiar?
It’s one of the most common stories women share when it comes to thyroid health. If I had known then what I know now, I could have addressed what’s called sub-clinical hypothyroidism long before it started impacting my hormones, energy, metabolism, and overall quality of life.
Here’s the reality: It often takes 10+ years for conventional medicine to finally recognize a thyroid problem. Even then, about 60% of people with hypothyroidism go undiagnosed their entire lives.
And in the meantime? Too many women are dismissed and told their symptoms are in their head. Or that their weight struggles have nothing to do with their thyroid — and everything to do with their fork. All while they continue to feel the exhaustion, brain fog, hair loss, and all the other classic signs of thyroid imbalance.
That’s why I’m sharing this with you today — so you have the tools to advocate for yourself and understand what’s really going on.
Here’s what we’ll cover together:
What are the key symptoms of Hypothyroidism
Why hypothyroidism is so commonly misdiagnosed
What tests you actually need to run
The difference between “normal” and optimal lab ranges
How to start making sense of your results
What to do if your doctor won’t run the labs you need
What are the Signs of Hypothyroidism or a Sluggish Thyroid?
Because thyroid hormone regulates metabolism, an under-functioning thyroid can impact nearly every cell and system in the body. This is why symptoms are often wide-ranging and, at times, surprising.
Hypothyroidism exists on a spectrum: in its mild form, it may cause only subtle issues, while in more advanced stages it can lead to debilitating effects. Interestingly, around 70% of women with hypothyroidism experience no obvious symptoms at all. Yet undiagnosed or untreated thyroid problems remains one of the primary reasons women have challenges getting or staying pregnant. It’s also a leading cause of hormone imbalances.
The most classic signs of an under-functioning thyroid are fatigue, hormone imbalances, fertility challenges, weight loss resistance and excessive hair shedding.
Here’s a broader look at symptoms that may appear:
Energy & Mood: fatigue, brain fog, poor focus, depression, anxiety, low motivation
Weight & Metabolism: unexplained weight gain, cold intolerance
Reproductive & Hormonal: irregular or heavy periods, PMS, low libido, fertility challenges
Hair, Skin & Nails: hair thinning/loss, brittle nails, dry skin
Digestive & Gut: constipation or sluggish digestion, bloating, food sensitivities
Cardiovascular: slow heart rate, low blood pressure
Muscles & Joints: weakness, stiffness, aches
Neurological & Sensory: dizziness, tingling, slowed reflexes
Other Signs: goiter or neck swelling, hoarseness, deepening voice
Why is hypothyroidism so commonly misdiagnosed?
If you’ve ever felt dismissed by a doctor despite having every symptom of thyroid imbalance, you’re not alone. Hypothyroidism is one of the most commonly overlooked conditions in women’s health.
There are three big reasons why hypothyroidism often slips through the cracks:
Incomplete lab testing
Inadequate lab ranges
Undiagnosed Hashimoto’s thyroiditis
Let’s break each one down.
1. Incomplete Lab Testing
In conventional medicine, thyroid testing usually stops at a single marker: TSH (thyroid stimulating hormone).
Here’s the problem:
TSH is not a thyroid hormone. It’s a signal from your brain to your thyroid, requesting that it produce thyroid hormones. But it doesn’t measure whether those hormones were actually made, converted, or delivered into your cells where they’re needed.
Only testing TSH is like sending out a work request and assuming the job is done without ever checking to see if anyone responded, showed up, or did the work correctly.
Here’s what really happens in the body:
TSH signals the thyroid to produce mostly T4 (thyroxine) and a little T3 (triiodothyronine).
T4 then needs to be converted into T3, the active thyroid hormone that powers your metabolism, energy, brain function, digestion, and more.
But sometimes conversion stalls. That means TSH and T4 look “normal,” while T3 — the hormone that actually matters — is too low.
Even more confusing, sometimes T4 is converted into reverse T3 (RT3). Reverse T3 looks almost identical to active T3, but it doesn’t work. The bigger issue? It binds to the same cell receptors as T3, blocking the real hormone from getting in.
Think of reverse T3 like putting the wrong key into a lock: it fits, but it won’t turn or open the door. And once it’s stuck there, the right key can’t get in either.
This is why testing only TSH (and sometimes T4) isn’t enough. Without looking at free T3 and reverse T3, you can be told your thyroid is “normal” when in reality, your cells are starved of usable thyroid hormone.
Why do some doctors believe TSH is enough?
Your thyroid and brain are connected through a deeply interconnected negative feedback loop. The brain releases TSH (thyroid-stimulating hormone) as a signal for the thyroid to produce more hormones. When the brain detects enough T4 or T3 in the blood, it suppresses further TSH production, signaling the thyroid to slow down.
However, there’s an important catch: the pituitary gland (which releases TSH) can “see” and respond to T4 almost as well as it does to T3, because it can convert T4 into active T3 for its own use. This means that even if the body’s overall T3 (the active, usable hormone) is low, a normal or high T4 level can still suppress TSH production. As a result, lab work can show “normal” TSH and T4, while T3 remains low and hypothyroid symptoms persist
So, relying on TSH (and sometimes T4) alone can miss cases where people don’t have enough of the hormone their body actually needs: T3, the true workhorse of thyroid health.
2. Inadequate Lab Ranges
Even when testing goes beyond TSH, there’s still a major issue: the lab ranges themselves.
Standard lab ranges are based on the average population — not the healthy population. In other words, the reference range includes people who already have thyroid dysfunction. As a result, your labs may not get flagged as “abnormal” until your thyroid dysfunction is severe, which is why it’s common for symptoms to go unrecognized for years. In fact, thyroid function can be declining for up to a decade before labs finally cross the “abnormal” line. In the meantime, symptoms like fatigue, brain fog, weight changes, hair loss, and constipation are often dismissed as stress, aging, or “just life”.
Instead of settling for results that are technically “normal,” we want to aim for truly optimal ranges — this is when people feel their best. More on what those lab ranges are and why they matter, coming up.
3. Hashimoto’s Disease: A Hidden Cause of Thyroid Problems
The third piece of the puzzle is Hashimoto’s disease, a common cause of hypothyroidism.
Hashimoto’s is an autoimmune condition where the immune system mistakenly attacks the thyroid gland, leading to inflammation and gradual thyroid damage. But here’s the tricky part:
Lab results can swing between hyperthyroid, hypothyroid, or even “normal” as the disease progresses.
Symptoms don’t always match the standard picture of low thyroid, and can be subtle, confusing or inconsistent because of those swings.
Standard thyroid testing often doesn’t check for Hashimoto’s.
This makes Hashimoto’s easy to miss.
The best way to test for Hashimoto’s is by running thyroid antibody tests:
Thyroid Peroxidase Antibodies (TPOAb)
Thyroglobulin Antibodies (TGAb)
These markers can show up years — even decades — before TSH becomes abnormal, giving you the chance to intervene earlier.
The Most Common Cause of Hypothyroidism:
Hashimoto’s disease is widely understood as the most common cause of hypothyroidism. However, I’ve observed many women experience subclinical hypothyroidism — a milder form of thyroid dysfunction but with many challenging symptoms — that isn’t driven by Hashimoto’s. Instead, it’s often linked to factors like emotional and physical stress, inadequate nutrition, chronic dieting, gut health issues, and/or liver problems.
Without addressing them, many women also gradually progress from subclinical to clinical hypothyroidism as their thyroid slows down more and more.
This highlights the importance of looking beyond autoimmune causes and focusing on whole-body health when assessing thyroid function and symptoms.
What thyroid labs should I have tested?
The good news is that hypothyroidism can be easily diagnosed if the right thyroid tests are ordered and interpreted with optimal lab ranges.
Here’s the comprehensive thyroid panel I recommend:
Thyroid Stimulating Hormone (TSH) – measures how hard your brain is pushing your thyroid to produce hormones.
Free T4 (FT4) – the main thyroid hormone produced, which serves as the storage form and needs to be converted into the active hormone (T3).
Free T3 (FT3) – the active hormone your body actually uses.
Reverse T3 (RT3) – the “look-alike” hormone that blocks real T3 from working.
Thyroglobulin Antibodies (TgAb) – helps detect Hashimoto’s.
Thyroid Peroxidase Antibodies (TPOAb) – another key marker for Hashimoto’s.
Important note: Make sure your doctor orders the Free T4 and Free T3 tests — not the Total T4 or Total T3. “Free” means the hormone is unbound and available for your cells to use. Bound hormones can look normal on labs but aren’t active in your tissues, which makes a big difference in how you feel.
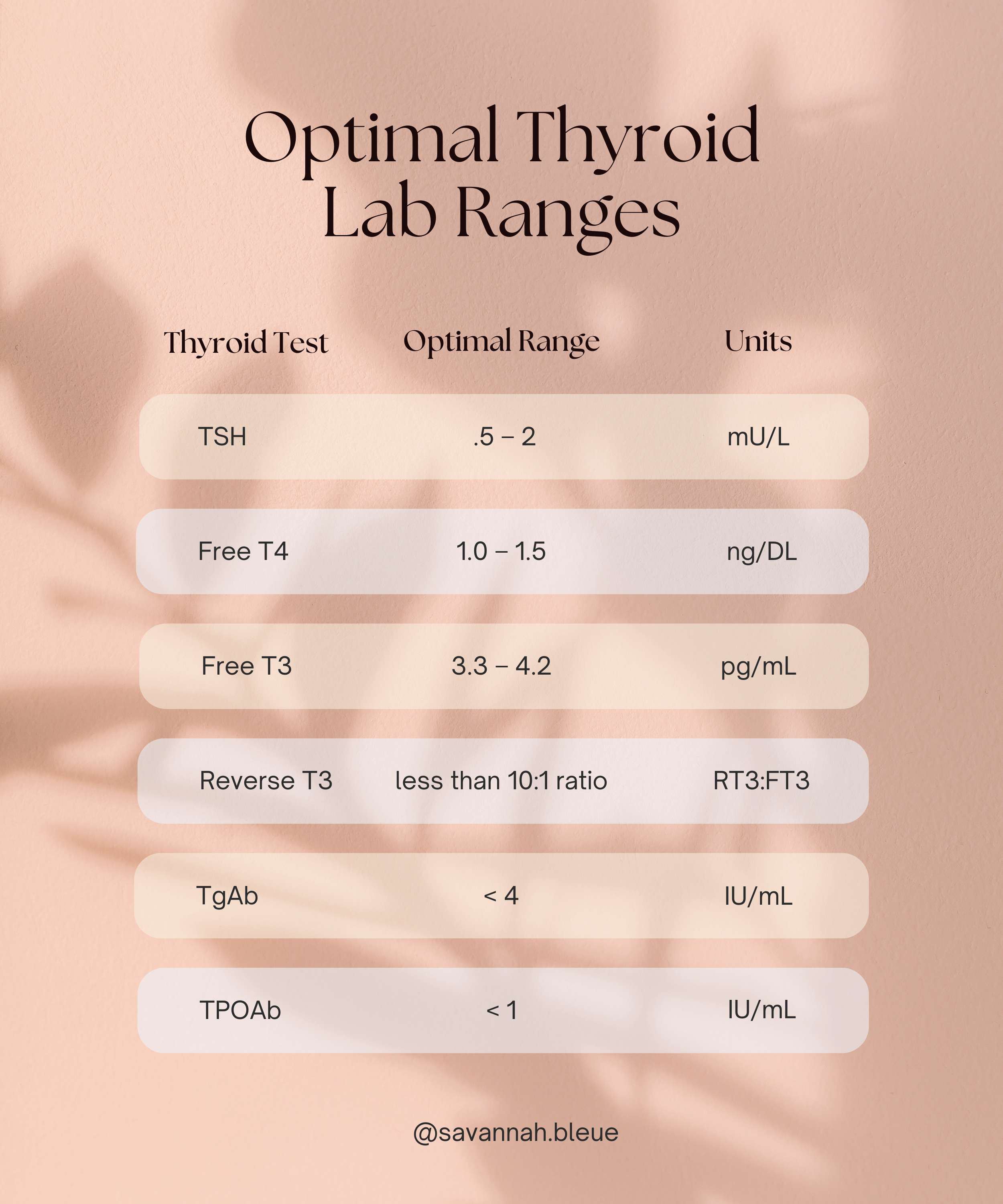
What are optimal lab ranges for thyroid hormones?
These ranges reflect numbers where patients typically report feeling their best.
TSH: .5-2 mIU/L.
Free T4: 1.0-1.5 ng/DL
Free T3: 3.3-4.2 pg/mL
Reverse T3: less than a 10:1 ratio RT3:FT3
Thyroglobulin Antibodies: <4 IU/mL
Thyroid Peroxidase (TPO) Antibodies: <1 IU/mL
What If Your Doctor Refuses to Run a Full Thyroid Panel?
Unfortunately, it’s common for this to happen. Doctors usually only order TSH (or sometimes TSH and T4), because that’s what’s considered standard.
One of the most helpful things you can do is go into your appointment prepared to advocate for yourself. Bring a list of your symptoms and share how they connect to thyroid health. If you can explain why complete testing would give you and your doctor more clarity, you’re more likely to get the labs you need.
If your doctor still isn’t willing or you don’t want to navigate that battle in the first place, you do have other options. Functional medicine doctors are usually much more open to running full panels and looking at optimal ranges. You can also work with a functional nutritionist who is authorized to run labs. The benefit of this route is that you not only get the testing, but also support to dig into the root cause of what’s happening with your thyroid, rather than focusing solely on medication or supplements.
If you’re curious about what this can look like, click here to learn more about working with me.
Hypothyroid Symptoms but Normal Labs? Here’s Why
Even if your bloodwork shows optimal T3 and T4 levels, you can still experience classic hypothyroid symptoms like fatigue, brain fog, hair thinning, or difficulty losing weight. This can happen due to cellular hypothyroidism, also called tissue-level resistance or impaired thyroid hormone transport.
Here’s what’s happening: inflammation, oxidative stress, insulin resistance, or toxic metabolites can interfere with thyroid hormone entering your cells or binding to receptors effectively. In other words, your cells are essentially starved of thyroid hormone even though your serum levels look normal.
This is why feeling “off” despite normal labs is more common than many realize. Bloodwork alone doesn’t always tell the full story — a closer look at inflammation, nutrient status, and overall metabolic health is often needed to uncover the root cause and restore proper thyroid function at the cellular level.
What Now? How to Support Your Thyroid
The path to thyroid health looks different for everyone. For some, medication is essential and life-changing, yet many women find they don’t feel completely better with medication alone. That’s because lasting thyroid health depends on a whole-body approach — supporting not just the thyroid, but also the gut, liver, and stress response, all of which play critical roles in hormone balance.
One common reason symptoms persist is that the standard thyroid medication, levothyroxine, contains only T4. If your body struggles to convert T4 into the active hormone T3, the medication by itself may not fully resolve symptoms.
In my own journey, I was able to restore thyroid health through diet and lifestyle adjustments alone. In my practice, I’ve also supported women who do take thyroid medication — helping them fine-tune nutrition, balance hormones, and optimize lifestyle so their medication works more effectively and they can finally feel like themselves again.
What I’ve seen time and again is that when you address the root causes and support the whole body, your thyroid and hormones have a much better chance of thriving.
If you’d like support with this, click here to book a free consultation. We’ll explore your symptoms, labs, and next steps together.
More Resources
Disclaimer: This information is for educational purposes only and is not intended to diagnose, treat, cure, or prevent any disease. It is not a substitute for personalized medical advice, diagnosis, or treatment. Always consult with your healthcare provider before making changes to your diet, supplement routine, or health practices. Full disclaimer here.