Understanding PCOS: What It Is, Why It Happens, and How You Can Heal
Polycystic Ovary Syndrome (PCOS) is one of the most common hormonal disorders women face, yet it’s still surrounded by confusion and misinformation. Being told you have PCOS can leave you wondering what it really means for your hormones, your cycles, and your fertility — so I want to start by saying this: PCOS is not a life sentence. Once you understand what’s happening in your body, there’s so much you can do to naturally rebalance your hormones, restore regular cycles, and start feeling like yourself again.
Let’s break it down together —
What is PCOS?
Polycystic Ovary Syndrome (PCOS) is a common endocrine disorder that affects women. It’s primarily a condition of androgen excess (high male hormones) and irregular or anovulatory cycles (lack of regular ovulation). High androgen levels interfere with follicle development and prevent regular ovulation, leading to symptoms such as:
Irregular or absent periods
Acne or oily skin
Excess facial or body hair (chin, upper lip, chest, belly)
Thinning scalp hair or male-pattern baldness
Weight gain or difficulty losing weight
Mood changes
Fertility challenges
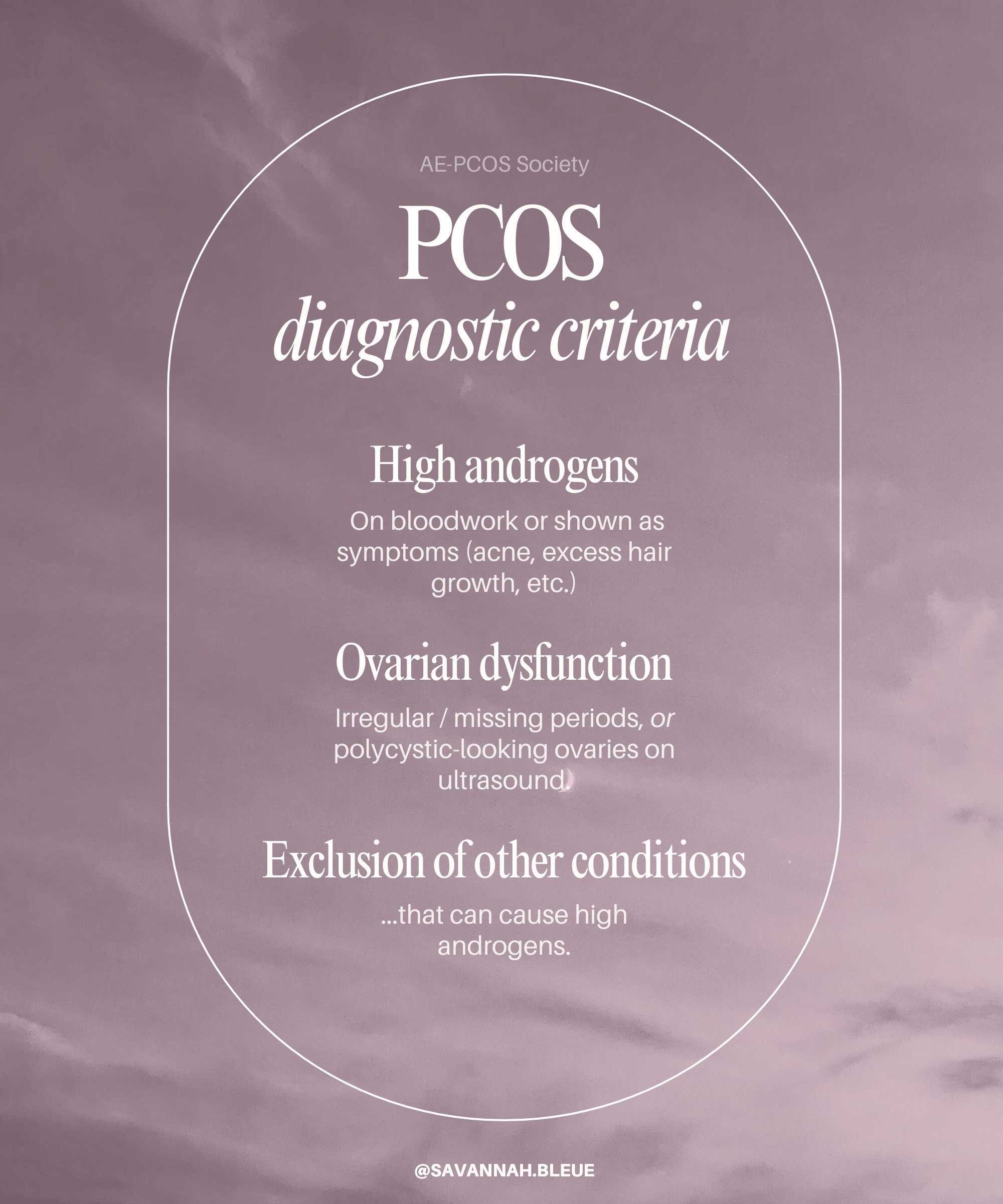
How is PCOS Diagnosed?
The most accurate way to diagnose PCOS is by the criteria outlined by the AE-PCOS Society — for a woman to have PCOS she must have all three of the following:
High androgens, shown either through symptoms (acne, excess hair growth, etc.) or confirmed by bloodwork.
Ovarian dysfunction (irregular or missing periods) OR polycystic-looking ovaries on ultrasound.
Exclusion of other conditions that can cause high androgens, such as thyroid disorders, high prolactin, Cushing's disease, or adrenal issues.
In other words, a true PCOS diagnosis requires both high androgens and either irregular cycles or polycystic ovaries.
Why does this matter? The Rotterdam criteria, used by most practitioners, allow a diagnosis of PCOS if you have just two of the following: irregular periods and polycystic ovaries — without the need for high androgens. This is problematic because many women with irregular cycles have polycystic ovaries for reasons that have nothing to do with PCOS.
Despite its name, you don’t need “cysts” on your ovaries to have PCOS.
Some women with PCOS have polycystic-appearing ovaries on an ultrasound, while others have normal-looking ovaries. Conversely, 25% of healthy women without PCOS can have polycystic ovaries show up on an ultrasound.
The term “polycystic ovaries” really just means ovaries that contain many small follicles.
If you have PCOS, it’s important to understand this. Let’s take a closer look…
How Follicles Develop and What Happens in PCOS
Each menstrual cycle, your ovaries start maturing multiple follicles — usually up to 12 developing follicles as an adult, and 25 as a teenager. Normally, as the cycle progresses, one follicle becomes dominant. This dominant follicle grows larger and eventually releases an egg during ovulation. This suppresses the other smaller follicles and then they’re naturally reabsorbed back into the body.
In PCOS or anovulatory cycles (where ovulation doesn’t happen), there is no dominant follicle to take over and suppress the others. As a result, many small follicles remain visible on the ovary. This creates the "polycystic" appearance on an ultrasound, which means the ovary looks like it has many cyst-like follicles.
It’s important to know that having polycystic ovaries doesn’t always mean you have PCOS—many women with irregular cycles but no actual PCOS show this pattern. Polycystic ovaries are a snapshot of follicles stuck in development, not the cause of PCOS itself.
Understanding this helps explain why just having polycystic ovaries and irregular periods without androgen excess does not mean a true PCOS diagnosis.
Types of PCOS and Common Drivers
Not all PCOS is the same. Each woman may have different underlying causes, and understanding yours is key to creating an effective, personalized approach to healing. According to Dr. Lara Briden, there are four main types of PCOS: insulin-resistant, inflammatory, adrenal, and post-pill. While this framework simplifies a complex condition — since many women experience a mix of root causes — it’s a helpful way to start identifying what’s driving your symptoms and where your body needs the most support.
The 4 Types of PCOS:
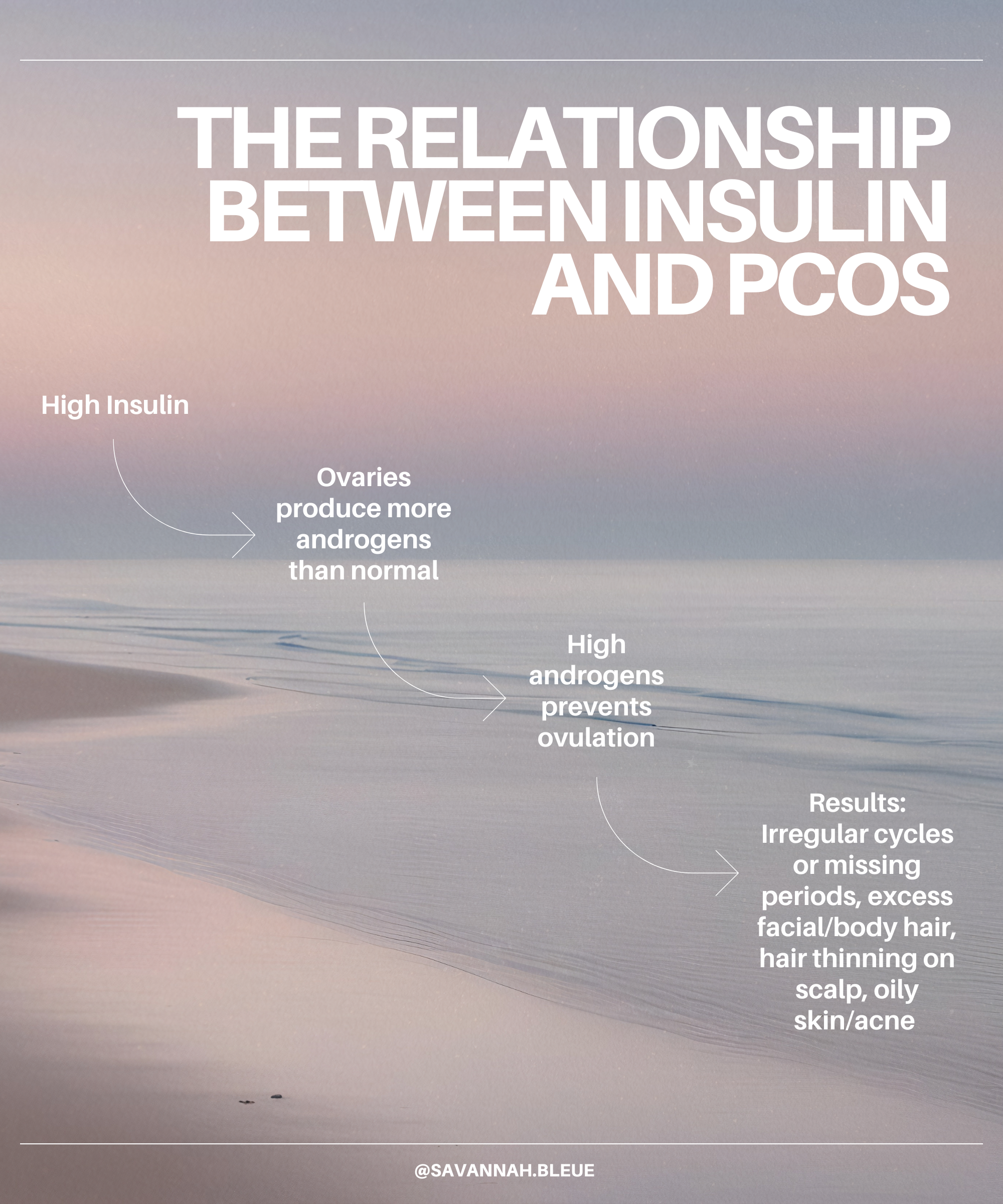
Insulin-Resistant PCOS: This is the most common type. High levels of insulin in the body can cause the ovaries to produce more male hormones (androgens). Most women with PCOS have some degree of insulin resistance, making this a common and central driver.
Inflammatory PCOS: Driven by chronic inflammation that disrupts hormone signaling and ovulation. Because inflammation and insulin resistance often influence each other, these two types frequently overlap.
Adrenal PCOS: In this type, the adrenal glands produce too much of the androgen hormone DHEA (and its sulfate form, DHEA-S). This isn’t as common as insulin-resistant PCOS and can sometimes be linked to chronic stress or how your nervous system is functioning. Importantly, it’s different from the ovarian androgen excess seen in other types and usually requires specific hormone tests to identify.
Post-Pill PCOS: Occurs after stopping hormonal birth control, when the body is recalibrating natural hormone production. When you stop the pill, your body needs time to adjust and restart hormone production. During this adjustment, there can be a temporary rise in testosterone and a delay in ovulation, which leads to symptoms like irregular or missing periods, acne, oily skin, and sometimes unwanted hair growth — as seen in PCOS. The pill may also increase insulin resistance and inflammation, key drivers in PCOS.
Factors That Can Make PCOS Symptoms Worse:
Poor Metabolic Health (Thyroid Function): A sluggish thyroid slows metabolism and disrupts many processes in the body, including ovulation. Approximately 25% of women with PCOS have hypothyroidism (an underactive thyroid).
Gut Dysbiosis: An imbalance of gut bacteria can contribute to inflammation, insulin resistance, and poor thyroid function.
Nutrient Deficiencies — Inadequate vitamins, minerals and amino acids can create a domino effect across multiple systems that support hormone production and function.
Stress — Chronic stress dysregulates blood sugar and can lead to insulin resistance and inflammation.
The Role of Epigenetics and Lifestyle
Epigenetics refers to how your environment and lifestyle influence how your genes express themselves — essentially turning certain genes “on” or “off” without changing your DNA.
In PCOS, factors like inadequate nutrition, high stress, and toxin exposure can “turn on” PCOS symptoms in genetically predisposed individuals. This doesn’t mean PCOS is your fault — but it does help explain why it can develop, even if you haven’t always had symptoms.
Here’s the hopeful part: once you understand the role of epigenetics, you realize that PCOS is modifiable. The same genes that were activated can quiet down as your environment and lifestyle change.
In other words, PCOS isn’t fixed or purely hereditary — your daily choices have the power to influence your hormones in a positive direction.
Can PCOS Be Reversed?
Because PCOS is influenced by epigenetics and lifestyle, it doesn’t have to be a permanent label. With the right support — nutrition, movement, stress management, and restorative habits — many women can significantly reduce or even eliminate their symptoms.
When you support your body with the nourishment and care it needs, hormones often rebalance naturally, cycles become more regular, and ovulation can return.
If symptoms resolve with these changes, it can be said that you no longer have active PCOS — a reminder that PCOS is a modifiable collection of imbalances, not a fixed or irreversible condition.
Will I Be Able to Get Pregnant?
It’s true that many women with PCOS experience difficulty getting pregnant — most often because ovulation isn’t happening regularly. But that doesn’t mean you can’t conceive, or that you’ll always face fertility challenges.
With the right support and a personalized approach, many women with PCOS go on to ovulate normally, conceive naturally, and have healthy pregnancies.
The key is understanding why ovulation isn’t happening. For some, it’s driven by insulin resistance; for others, chronic stress, inflammation, or hormone changes after stopping birth control play a role. Once those underlying factors are addressed and ovulation resumes, fertility usually follows.
So if you’ve been told that PCOS means you’ll struggle to get pregnant — take heart. PCOS does not equal infertility. When hormones rebalance and ovulation returns, your body can absolutely do what it was designed to do.
Why Birth Control Isn’t a Solution for PCOS
It’s incredibly common for women with PCOS to be handed a prescription for birth control as the “solution” to their symptoms. Irregular periods? Birth control. Acne? Birth control. Excess hair growth? Birth control.
But here’s the problem: birth control doesn’t fix PCOS. It simply shuts down your natural hormonal rhythm.
When you’re on the pill, the bleeding you experience each month isn’t a real period. It’s a withdrawal bleed, triggered by the sudden drop in synthetic hormones during the placebo week. There’s no true ovulation happening and that’s important because a lack of ovulation is one of the core issues in PCOS.
So when we use a drug that prevents ovulation to “treat” a condition defined by the absence of ovulation, it doesn’t make much sense, does it?
Birth control can help manage certain symptoms in the short term, like regulating bleeding or improving acne, but it doesn’t address the root causes such as insulin resistance, inflammation, or stress-related hormone imbalances. And once you stop taking it, those symptoms often come right back because the underlying dysfunction hasn’t been resolved.
If you truly want to heal PCOS, the goal isn’t to suppress your natural cycle — it’s to support your body back into balance so ovulation can return naturally. That’s where lasting change and real hormonal health begin.
And if you do want to get pregnant one day, it’s important to address your PCOS rather than suppress it with birth control — because that brings you further away from restoring ovulation and a healthy cycle, not closer.
The Takeaway
If you’ve been diagnosed with Polycystic Ovary Syndrome (PCOS), know this: your body isn’t broken—it’s communicating. Every symptom is information, showing you where your body needs hormonal support, nourishment, and rest to come back into balance.
By understanding your unique drivers of PCOS and addressing the root causes — like insulin resistance, inflammation, or stress — you can restore ovulation, balance your hormones naturally, improve energy and mood, and feel empowered in your fertility journey.
Healing PCOS isn’t about perfection—it’s about connection, consistency, and compassion for your body as it finds its way back to natural hormonal balance.
Start Healing the Root Causes of PCOS — Not Just the Symptoms
If PCOS or any hormone imbalance is affecting your energy, cycles, or fertility, know that you don’t have to navigate it alone. The right support can help your body find its rhythm again, bringing balance to your hormones and relief to your symptoms.
As a nutritionist specializing in women’s hormone health, I help women uncover what’s really driving their symptoms and create sustainable, nourishing changes that support healthy ovulation, balanced moods, and steady energy.
Together, we’ll design a personalized plan that meets your body where it’s at—helping you feel grounded, clear, and confident in your health again.
✨ Book your free 15-minute consultation to learn how we can work together to restore balance and vitality from the inside out.